Hamstring Strains in Sports
Dr. Luga Podesta / St. Charles Orthopedics
Dr. Luga Podesta is a non-operative orthopedic sports medicine specialist. Dr. Podesta has joined the Sports Medicine Team of physicians at St. Charles Orthopedics.
For More info. contact Dr. Podesta @ 631-689-4184. Dr. Podesta is seeing patients at St Charles Orthopedic offices in East Setauket, Patchogue and Commack.

Coach My Elbow Hurts
By Luga Podesta, M.D
Baseball and softball season is upon us, and with every new season come increasing numbers of young players developing elbow pain. Elbow pain is the most common complaint I am asked to evaluate in young throwing athletes. Unfortunately, the number of little leaguers, middle school and high school players I am evaluating for elbow pain has risen tremendously over the last few years. I attribute this to a number of problems. First, these young athletes are asked to throw more than their maturing muscles and bones can handle. Second, they do not get adequate rest after throwing to allow their muscles, ligaments and bones to recover. Third, they are either taught, or on their own, try to throw pitches that their bodies are not developed enough to throw properly. One or a combination of all these factors can contribute to the development of significant elbow problems. Players, Parents and Coaches must be familiar with the early warning signs. The injuries will be different depending on the age and skeletal maturity of the young player.
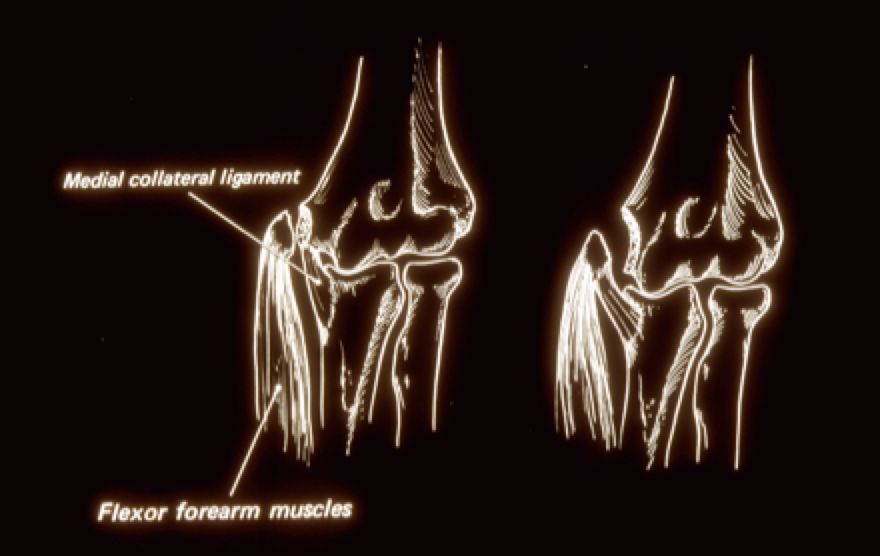
There are a number of problems that can occur in the young throwers elbow. The most common injury to the younger skeletally imature throwers elbow is Little Leaguer’s Elbow. Little Leaguer’s Elbow is actually an injury to a growth plate on the inside (medial) portion of the humerus bone in a skeletally immature child. Little Leaguer’s Elbow results from either a chronic stress to the growth plate or from a sudden pull on the growth plate by the muscles and tendons that attach to it (Figure 1).
These young athletes will frequently present with complaints of elbow pain and swelling localized to the inside or medial portion of the elbow. They will often complain of loss of elbow motion, numbness, tingling, pins and needles sensation in the hand. When they attempt to throw, they will find they have a loss of velocity of their throws and they have lost control of their throws.
The diagnosis of Little Leaguer’s Elbow is usually quite easy. The young prepubescent (skeletally immature) athlete will have tenderness at the medial humeral growth plate. This can be made worse with stretching the muscles that attach there.
Evaluating, and comparing, radiographs of both the injured and non-injured elbows confirm the diagnosis of Little Leaguer’s Elbow. Radiographs will show a separation of the medial humeral epicondyle (Figure 2).

The treatment of Little Leaguer’s Elbow requires the athlete to stop all throwing activity, allowing the bone to heal. Since this is actually a fracture of the growth plate, treatment is similar to the treatment for most other fractures. Treatment initially will involve immobilizing the elbow for 2 to 6 weeks in a sling. After this short period of immobilization and before throwing can begin, a course of physical therapy including range of motion exercises and strengthening of the shoulder, elbow and core musculature begins. Throwing does not begin until the fracture has healed and therapy is completed. A progressive interval-throwing program is not started until the elbow is pain free, range of motion is complete, radiographs reveal a healed fracture, and the arm is strong.
Occasionally surgical treatment is necessary to repair the fracture. Surgery is indicated when the growth plate is significantly separated from the humerus bone.
When elbow pain develops in the young throwing athlete, it is extremely important to have the elbow evaluated. It is not sufficient to take a wait and see approach hoping the elbow pain will disappear. The majority of the time it is NOT just a sprain. If the underlying cause of the injury is not discovered or corrected, the risk of re-injury or permanent damage to the growth center is significant. Remember Kids Don’t Sprain They Break!
There are a number of warning signs of elbow injury that must be recognized:
1. Pain in the elbow
2. Loss of elbow motion
3. Loss of control
4. Loss of velocity
5. Swelling of the elbow
6. Inability to warm up
7. Numbness, tingling, pins and needles sensation in the hand
 Dr. Luga Podesta, M.D.
Dr. Luga Podesta, M.D.
Dr. Podesta is a nationally recognized sports medicine physician specializing in the non-surgical treatment of orthopedic, musculoskeletal and sports-related injuries to the shoulder, elbow, knee, and spine, and brings with him a wealth of experience on and off the field. He is considered a pioneer in the new field of regenerative medicine, an area of medicine with the potential to fully heal damaged tissues, offering hope for individuals who are unable to or do not choose to undergo surgery. Dr. Podesta is the medical director and head team physician for the Los Angeles Kiss (Arena Football League) and served as team physician for the Los Angeles Angels Baseball team (2010-2013) and the Los Angeles Dodgers (1990-2006.) He also served as head team physician for the World Champion LA Xtreme (XFL) (2001,) the Los Angeles Avengers, AFL (2002-2008) the Los Angeles Riptide MLL (2006-2008,) Oxnard College, and as team physician for Loyola Marymount University.
Mechanical Low Back Pain
By Dr. Danielle DeGiorgio, DO, FAAPMR
What is it?
Mechanical low back pain is a term given to back pain that has multiple causes. The back is made up of many different parts including bones, joints, ligaments, muscles, discs and nerves. These structures offer mechanical strength and protection as well as flexibility to move the extremities freely. If the alignment and movement patterns of these structures become abnormal, injury may ensue. These less than ideal movement patterns can develop from poor posture, weak core musculature, improper training, muscle imbalance, overuse, and/or deconditioning.
Symptoms
As the cause is multifactorial, patients’ symptoms may vary. However, a localized lower back pain is most commonly described. This pain can be dull or sharp and can present before, during or after activity. Immediate attention is required if there is motor (paralysis, weakness) or sensory (numbness, tingling) changes in the legs or changes in bowel and/or bladder function.
 Dr. Danielle DeGiorgio, DO
Dr. Danielle DeGiorgio, DO
Sports Medicine Evaluation/Treatment
A sports medicine evaluation will include a thorough history of the event/events that led to the injury, followed by a neurologic and musculoskeletal physical examination.
Unfortunately, there is no specific test for mechanical low back pain. However, further testing/imaging can be completed to rule out other diagnoses that may present with similar symptoms.
The goals of treatment for mechanical low back pain are to reduce patient discomfort, improve function and prevent future injury.
Initial evaluation includes identifying weakness, abnormal patterns and postures, which may be causing tissue overload and pain. Correction of these abnormalities can be completed in a progressive manner starting with a more general approach (core strengthening, stabilization and motor control exercises) followed by an advanced sport’s specific training.
Adjunctive treatment options that have also been proven to be helpful include anti-inflammatory medications, therapeutic modalities (heat, ice, electrical stimulation, etc), manual therapy and acupuncture.
Injury Prevention
As the majority of movement stems from the spine, proper technique and training prior to competition is extremely important. This should begin by creating a strong foundation of core musculature, development of proper body posture and mechanics, which can then be enhanced by a more sport’s specific training program.
Return to Play
Athletes can return to play when they have full, painless range of motion and strength, and can complete all portions of their sport (cutting, jumping, running) without symptom development.
Danielle DeGiorgio, DO, is a native of Long Island, graduating from Longwood High School as a three-sport athlete. She attended Stony Brook University on a full athletic scholarship and served as captain of the women’s basketball team. After obtaining her medical degree from New York College of Osteopathic Medicine, Dr. DeGiorgio completed an internship at Brookhaven Memorial Hospital, followed by a residency in Physical Medicine and Rehabilitation (PM&R) at Stony Brook University Medical Center, serving as chief resident in her senior year. In addition, Dr. DeGiorgio completed training in structural acupuncture at Harvard Medical School.
Rainouts, too many games and not enough arms!
By Luga Podesta, M.D.
It is the early spring on Long Island and the high school baseball season is in full swing. Unfortunately, with spring comes rain and rained out high baseball games. With a short high school season and a predetermined playoff schedule, rained out games need to be made up. This can become a recipe for disaster to a team’s pitching staff. If teams are placed in a position where they might have to play 6 games in 7 days, these pitchers are asked to subject their arms to potential injury!
Most states have rules regarding how much a high school pitcher can pitch in any given week, New York does not!
New Jersey for example limits innings pitched and days rest:
• A pitcher may not appear as a pitcher again for three (3) calendar days after
having pitched six (6) or more innings on any day.
• A pitcher may not appear as a pitcher again for two (2) calendar days after having
pitched five (5) innings.
• A pitcher may not appear as a pitcher in more than a total of ten (10) innings
during any (4) calendar day period. This does not set aside 1 or 2 above.
California on the other hand restricts overall number of pitches:
1. Sections shall adopt the following baseball pitching limitation rule: 30 outs and/or three appearances in a calendar week.
a. The calendar week begins Monday.
b. Innings pitched in a no game (i.e. rainout, power failure, etc.) shall count toward the total.
c. If the 30th out involves a double or triple play, the team will not be penalized.
d. An appearance is defined as a pitcher pitching at least one pitch. If the pitcher is removed from the mound to another position or to the dugout, and later returns to pitch in the same game, the pitcher will be charged with a second appearance.
e. Any violation constitutes a forfeit of the contest.
So what’s the solution? This can be a difficult problem for most HS teams to solve especially when pitching staffs are limited; there is no time for adequate rest and game need to be played.
Possible solutions to this dilemma might be:
1) Spread out the rained out games over a longer period of time.
2) Limit innings pitched per game to (4-5) innings, allowing the pitcher to appear again in two (2) calendar days.
3) Limit the total number of pitches for 15-18 year old players to 40-60 pitches per game followed by a mandatory 2 days rest.
4) Substitute a JV pitcher or pitchers in the normal varsity rotation to allow for necessary rest periods for pitching staff or to help spread out the number of innings pitched over a larger number of pitchers.
5) Prohibit a pitcher to substitute as a catcher and visa versa in the same game.
6) Be aware of the number of innings a catcher plays per game and games played per week. Alternate catchers when your catcher begins to exhibit any signs of fatigue.
(They are throwing just as much as a pitcher!)
 Dr. Luga Podesta, M.D.
Dr. Luga Podesta, M.D.
Dr. Podesta is a nationally recognized sports medicine physician specializing in the non-surgical treatment of orthopedic, musculoskeletal and sports-related injuries to the shoulder, elbow, knee, and spine, and brings with him a wealth of experience on and off the field. He is considered a pioneer in the new field of regenerative medicine, an area of medicine with the potential to fully heal damaged tissues, offering hope for individuals who are unable to or do not choose to undergo surgery. Dr. Podesta is the medical director and head team physician for the Los Angeles Kiss (Arena Football League) and served as team physician for the Los Angeles Angels Baseball team (2010-2013) and the Los Angeles Dodgers (1990-2006.) He also served as head team physician for the World Champion LA Xtreme (XFL) (2001,) the Los Angeles Avengers, AFL (2002-2008) the Los Angeles Riptide MLL (2006-2008,) Oxnard College, and as team physician for Loyola Marymount University.
The 6 Most Common Running Injuries
By Danielle DeGiorgio, DO, FAAPMR
 Dr. Danielle DeGiorgio, DO
Dr. Danielle DeGiorgio, DO
1) Hamstring Strain: The hamstring is a large muscle group in the posterior thigh, connecting the hip and knee. Symptoms may start as reoccurring tightness, but may progress to sharp debilitating pain. It is caused when the muscle is overstretched leading to a partial or complete tear.
2) Achilles Tendinopathy: The Achilles is a large tendon that connects the calf muscles to the heel. Symptoms include pain in the back of the ankle/heel, which can present as stiffness in the morning or severe pain with running. It is caused by overuse and inflexibility.
3) Plantar Fasciitis: The plantar fascia is found on the sole of the foot. Symptoms include sharp heel pain worse with the first step in the morning and/or with prolonged standing. It usually occurs with increased stress on the fascia, exacerbated by inflexibility or abnormal foot/ankle biomechanics.
4) Medial Tibial Stress Syndrome aka Shin Splints: Symptoms include shin pain that increases with activity. It is caused by repetitive bony overload of the tibia or shin bone. If left untreated, shin splints may progress to a stress fracture.
5) Iliotibial Band Friction Syndrome: The iliotibial (IT) band begins at the outside (lateral) hip and crosses the lateral aspect of the knee. It is a common cause of sharp lateral knee pain in runners. This is due to friction between the IT band and lateral femoral epicondyle (located just above the knee), which leads to inflammation in this area.
6) Patellofemoral Syndrome aka Runner’s Knee: Symptoms include pain around or behind the kneecap (patella). It is caused by friction due to poor tracking of the patella within the naturally occurring groove in the thigh bone (femur).
Injury Prevention:
Injury prevention begins with proper nutrition, hydration, and sleep. Additionally, athletes can follow these general guidelines to reduce the above overuse injuries:
1) Keep core and gluteal muscles strong
2) Maintain muscle flexibility (especially hamstrings, hip flexors, calves)
3) Do not increase mileage more than 10%/wk
4) Do not abruptly change distance, surface, and/or intensity of workout
5) Replace running shoes every 3-6 months or 200-300 miles
6) Remember to allow for recovery time
Treating Injuries:
The general principles behind treatment include:
1) Reducing pain and inflammation
2) Restoring full painless range of motion
3) Regaining full strength and endurance
4) Progression to sports specific movement/agility
5) Prevention of future injury
The bottom line: Injuries are a part of sports. As a former 3-sport high school athlete and a Division 1 collegiate basketball player, I know how important it is to stay in the game. It is vital that athletes don’t let their fear of being held out of competition, prevent them from being evaluated and treated. Subtle pain can lead to a decrease in muscle activation and peak performance. Therefore, letting a “minor” injury go untreated can lead to more serious complications. As a Sports Medicine Physician, it’s my job to keep athletes competing at their highest level.
Danielle DeGiorgio, DO, is a native of Long Island, graduating from Longwood High School as a three-sport athlete. She attended Stony Brook University on a full athletic scholarship and served as captain of the women’s basketball team. After obtaining her medical degree from New York College of Osteopathic Medicine, Dr. DeGiorgio completed an internship at Brookhaven Memorial Hospital, followed by a residency in Physical Medicine and Rehabilitation (PM&R) at Stony Brook University Medical Center, serving as chief resident in her senior year. In addition, Dr. DeGiorgio completed training in structural acupuncture at Harvard Medical School.
Concussion Baseline Testing
By Mark Harary M.D. / Published March 28, 2016
Baseline testing has become an important tool in the management of concussions. Many school districts and sport leagues conduct baseline testing on their athletes. Despite that, there can be a lot of confusion as to what exactly “baseline testing” is and how it can be helpful. A baseline test tries to measure how people perform on certain tasks under normal circumstances. This can then be compared to performance after an injury to see where deficiencies are, and to help guide treatment plans.
 Dr. Mark Harary, MD
Dr. Mark Harary, MD
What makes a good baseline test? A good baseline test is one that can be administered to large groups of people within a short amount of time and produces valid, reliable and repeatable results. Several companies that have created baseline tests but the most popularmis the Impact test. Impact is a computer based test that is typically completed in about 20-25 minutes. Test takers complete several cognitive tasks as quickly and accurately as they can. Based on performance on these tasks, an athlete’s baseline score is determined. After a head injury, this test is repeated to see how post-injury performance compares to the pre-injury baseline.
Who should have a baseline test? Anyone that participates in a sport with a high risk of concussion, should have a baseline test. However, this is not always a possibility. Some tests cannot be performed on certain populations. For example, the Impact test is validated for use between the ages of 11 and 60 years. Outside of that range, we can’t be sure that the test results accurately measure the test taker’s cognitive abilities. Also, people with learning disabilities or vision problems would possibly have a difficult time taking this type of test even when performing at their best. It is important to get a good night sleep prior to taking a baseline test because this can affect performance. It should not be done immediately after practice or games, or during any other potentially stressful or distracting situations.
How is baseline testing used? While a baseline test is done prior to an injury, the same test is performed after a concussion to look at post-injury performance. We then look at differences between the two tests. Decreased performance on memory sections of the test may indicate that the athlete needs schoolwork or testing limitations. If reaction time is slowed, that indicates that the athlete should avoid contact sports and possibly driving as well. As healing of the injury occurs, testing can be repeated to ensure a return to baseline performance.
What are the limitations? Baseline testing has limitations. Impact testing, as mentioned earlier, is not a reliable test for kids younger than 11 years old. Because it is often done in groups, there is the potential for distractions affecting performance. Finally, in rare instances, athletes may try to intentionally do poorly on the test in hopes of getting back on the field sooner.
In conclusion, baseline testing can be a very useful tool in concussion management, when applied to the right situation.
Dr. Harary earned his undergraduate degree in Movement Science from the University of Michigan in 1998. He went on to medical school at Ross University, where he graduated with honors in 2002. After obtaining his medical degree, Dr. Harary completed a family medicine residency at UPMC Shadyside Hospital in Pittsburgh, PA. He then completed his fellowship training in Sports Medicine at Blessing Hospital in Quincy, IL. Dr. Harary is board certified in Sports Medicine and Family Medicine. He is a member of the American Medical Society of Sports Medicine and the American Academy of Family Physicians. Dr. Harary is actively involved with the Arthritis Foundation. He has given numerous educational talks on arthritis and has served on the planning committee for the annual Arthritis Walk for several years, serving as the Walk Chair for the NYC Arthritis Walk in 2014.
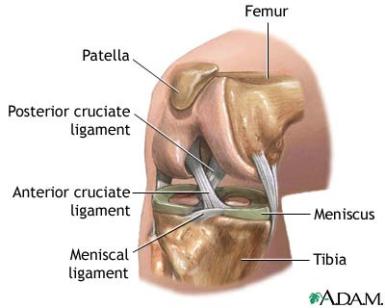
Anterior Cruciate Ligament Injuries
By Michael J. Sileo, MD, FAAOS / Published March 20, 2016
The anterior cruciate ligament (ACL) is one of the major stabilizing ligaments in the knee. It is a strong, rope-like structure located in the center of the knee, connecting the femur (thigh) bone to the tibia (shin) bone. The ACL prevents the tibia from moving abnormally on the femur. When the ACL tears, it does not heal. This leads to instability of the knee, which limits the ability to perform cutting and pivoting activities frequently required to participate in sports.
Most ACL injuries are sports related. It can occur with a sudden change in direction, twisting, or landing awkwardly. The vast majority of ACL tears are “non contact”, and 75% of patients report hearing or feeling a “pop”. Swelling is common almost immediately, and most athletes cannot continue to play after the initial injury. Diagnosis is typically made by an athletic trainer, physical therapist, or orthopedic surgeon based on the history, physical examination, and imaging including x-rays and MRI.
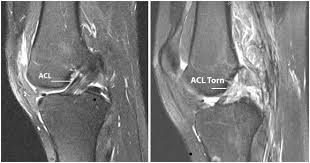
Treatment for athletes who sustain an ACL tear initially focuses on “RICE”, Rest, Ice, Compression, and Elevation. The Sports Medicine Department at St. Charles recommends aggressive treatment of the swelling with a prescription strength anti inflammatory pill. Additionally, we recommend early commencement of a “Pre-hab program” with a sports medicine trained physical therapist to work on early range of motion, isometrics to maintain the quadricep muscle, along with modalities to help minimize swelling.
 Michael J. Sileo, MD, FAAOS
Michael J. Sileo, MD, FAAOS
Most athletes who wish to return to sports will require surgery to reconstruct their ACL. It is important to remember that no two ACL tears are the same. Every athlete has different goals which must be taken into consideration when making important decisions about their reconstructive surgery. The type of graft used to reconstruct the ACL may vary depending on the age, demand, and sport of the particular athlete. In addition, the timing of surgery, anesthesia type, existence of other cartilage injuries, and bracing options all must be considered when planning the procedure.
ACL reconstruction is performed arthroscopically (using a video camera and very small incisions), and patients typically go home from surgery the same day. Walking on the knee is encouraged, with a knee brace. The importance of an organized and systematic rehabilitation program is crucial to the athlete’s short and long term outcome. The St. Charles Sports Medicine ACL protocol calls for early focus on range of motion, modalities to limit swelling, and isometric exercise that allows the athlete to strengthen without injuring their new ACL. As range of motion increases, focus progresses to strengthening, endurance, and ultimately sport specific activity. Current recommendations allow for return to full sport at 6-9 months, depending on the level of athletic participation.
Dr. Sileo is Board Certified – Orthopedic Surgery and Sports Medicine and St. Charles Orthopedics, Division of Sports Medicine.
Avoiding Tommy John surgery and UCL injuries
By Luga Podesta, M.D. / Published March 13, 2016
Every year about this time I begin to see in my practice young high school throwing athletes that develop pain in their elbows. I have had to oppurtunity to treat baseball players at every level of the game and have spent the last 20 plus years serving as a MLB team physician and consultant. Unfortunately, I have been forced to treat young throwers with injuries that I typically wouldn’t have seen until they reached collegiate or professional baseball. In fact, over the past 5 to ten years, there has been an epidemic number of young throwers injuring their Ulnar Collateral Ligament (UCL). The UCL is the major stabilizing ligament of the elbow and when injured, it becomes very difficult to throw effectively and painlessly.
Studies have shown that the throwing athlete, specifically pitchers are at significant risk of injury when throwing with arm fatigue. If the pitcher throws greater than 80 pitches per game, they are 4 times at risk of having elbow surgery. If that athlete pitches competitively for greater than 8 months per year they have a 5 times likelihood of elbow injury. If they pitch regularly with a fatigued arm, they are 36 times as likely to have an injury and potential need for surgery.
 Dr. Luga Podesta, M.D.
Dr. Luga Podesta, M.D.
Pitching while fatigued, pitching too many innings/year, not enough rest from throwing at end of the season, too many pitches per game, per week, per year, pitching consecutive days and playing on multiple teams & leagues at the same time are all associated risk factors for developing a UCL injury. These injuries can be prevented if we watch for and respond to signs of arm fatigue, stop all overhead throwing of any kind for at least 3-4 months/year (4 months is preferred), do not paticipate in competitive baseball pitching for at least 4 months/year, limits pitch counts and days rest dependent on age, avoid pitching on multiple teams, and practice good throwing mechanics. Remember - if your arm hurts STOP THROWING and seek a medical evaluation by someone that understands the throwers elbow.
Treatment for UCL injuries has been drastic. Tommy John Reconstruction which is a surgical procedure to replace the injured ligament requires a surgeon that is experienced in performing this procedure and 14 to 18 months of rehabilitation prior to returning to play. Unfortunately, amongst the baseball community several myths have arisen and are circulating regarding this surgery. There are significant risks involved with Tommy John surgery and it is absolutely NOT TRUE if someone tells you that you will throw harder, that the new ligament is better than the original ligament, that the surgery should be performed to enhanced pitching performance, your pitch speed will improve, surgery is always successful or that you will retun in 1 year.
Over the past several years, we have developed that capabilities to heal the UCL without surgery enhancing our bodies inate regenerative capabilities by injecting the injured ligament with concentrated platelets-Platelet-Rich Plasma (PRP) or Stem Cells. The healing time is significantly less that surgery, 10 to 14 weeks, is as successful and is performed in the office setting.
There are a number of warning signs that must be recognized that may signal a UCL injury including:
1. PAIN IN THE ELBOW OR FOREARM
2. LOSS OF ELBOW MOTION
3. LOSS OF CONTROL
4. LOSS OF VELOCITY
5. SWELLING OF THE ELBOW
6. INABILITY TO WARM UP
7. NUMBNESS, TINGLING, PINS AND NEEDLES SENSATION IN THE ARM AND/OR HAND
UCL injury can be a career ending for the throwing athlete. Don’t let it happen to you. The only one that WILL protect your arm is YOU. If your elbow begins to hurt, STOP THROWING and get it checked out by a physician.
Dr. Podesta is a nationally recognized sports medicine physician specializing in the non-surgical treatment of orthopedic, musculoskeletal and sports-related injuries to the shoulder, elbow, knee, and spine, and brings with him a wealth of experience on and off the field. He is considered a pioneer in the new field of regenerative medicine, an area of medicine with the potential to fully heal damaged tissues, offering hope for individuals who are unable to or do not choose to undergo surgery. Dr. Podesta is the medical director and head team physician for the Los Angeles Kiss (Arena Football League) and served as team physician for the Los Angeles Angels Baseball team (2010-2013) and the Los Angeles Dodgers (1990-2006.) He also served as head team physician for the World Champion LA Xtreme (XFL) (2001,) the Los Angeles Avengers, AFL (2002-2008) the Los Angeles Riptide MLL (2006-2008,) Oxnard College, and as team physician for Loyola Marymount University.